Technology and Predictive Analytics: Navigating Cardiovascular Risk - Part 2
Background
In Part 1, I covered the following:
What is a Cardiovascular disease?
How are these diseases diagnosed currently?
Can a combination of high-quality datasets, traditional clinical algorithms & machine learning be a possible solution?
A comprehensive understanding of the human body, even when focusing on a single condition like CVD, presents two main obstacles.
How to monitor the human body and the frequency of monitoring?
Gathering pertinent information about the human body given that it is an incredibly complex and dynamic system.
I will be covering the above two topics in this blog post in the context of CVD.
Monitoring the human body
Tech companies like Netflix, and Uber can monitor thousands of servers in real-time using tools such as CloudWatch, DataDog or through homegrown observability stack, without you noticing a blip while watching Narcos or while hailing a ride to work during peak hour. A dozen parameters such as CPU, Memory, IO, latency and so on might suffice to monitor a bazillion servers. (I am greatly simplifying to get the point across).
However human biology is different. Human beings are not like Docker containers starting with a pristine state. There is a lottery called genetics that plays an outsized role in the health of an individual. Lifestyle, environment and nutrition complicate the matter further. The inherent intricacies of biology, ethical considerations, invasive nature of data collection and technical challenges all make it a very complex endeavor.
Let's go back to the CVD example...
Historically patients were subjected to tests like ECG if a physician suspected an underlying cardiac problem and wanted to be sure. This provides a "point in time" snapshot of the patient's condition. (Kind of like capturing the server metrics during peak hour instead of monitoring it continuously)
However, a condition like Arrhythmia discussed in Part 1 might not manifest during a routine ECG test. So the Cardiologist might request the patient to wear a Holter Monitor. Holter monitors enable continuous tracking of the heart's electrical activity over several days. This extended monitoring provides a more comprehensive and accurate understanding of the heart's condition.
Consumer devices such as the Apple Watch can now measure ECG, and detect Arrhythmia with high accuracy. (Apple Watch has received FDA clearance.)
However, each of the above options has a trade-off between cost, turnaround time for results, accuracy, administrative burden and patient experience.
And we are just talking about one parameter! (Electrical activity of the heart). A physician has to consider other variables such age of the patient, gender, smoking habits, presence of high blood pressure and so on.
This leads us to the second problem...
Making sense of the data
Say Mr Doe has chest pain, and fatigue and is feeling dizzy. In India, the common practice is to consult a family doctor or a local clinic in the vicinity.
During this visit, the doctor will enquire about Mr. Doe's age, and symptoms and write down the clinical assessment on a sheet of paper.
The medicines are also prescribed on paper.
In certain instances, the doctor might request blood work. In this scenario, Mr. Doe would head to a nearby diagnostic center. Subsequently, the lab would either send back the results as a PDF file via email or furnish a printed copy of the blood report.
Regrettably, if Mr. Doe's condition worsens and he seeks assistance from a Cardiologist at a multi-specialty hospital, the Cardiologist faces the challenge of sifting through stacks of paper records. Within a limited half-hour window, the Cardiologist must converse with the patient about their present state and swiftly determine the subsequent steps to take. (The physician-to-patient ratios in India are very low, causing a strain on overburdened trained medical professionals.).
Could this solution work?
Take a picture of the handwritten paper documents or upload digital documents (such as PDF or Word files) using a custom-built Patient Mobile App that leverages OCR (Optical Character Recognition) capabilities provided by Amazon (Textract), Google (Document AI) or other players like Docsumo.
Here is an image of a sample blood report fed to Google Document API and the results...

Generally with handwritten documents, the results of OCR APIs are not as good. (Given that handwriting is so varied). Here is one example from Google Document AI ...
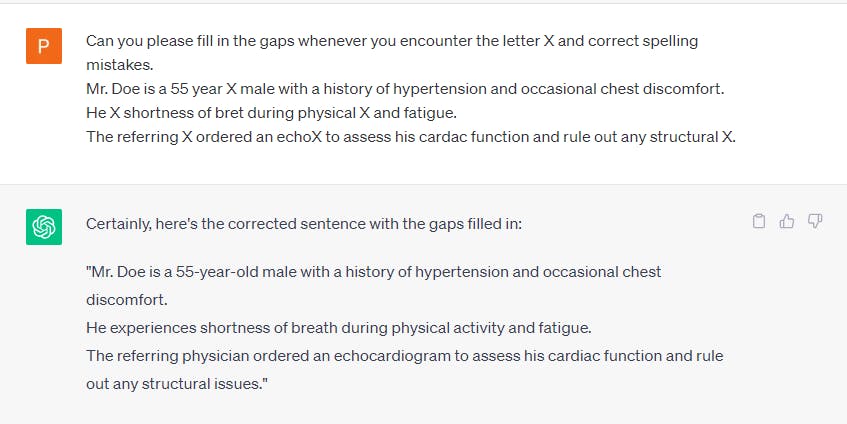
3. This is where LLMs can help. When text with inaccuracies and missing bits are fed to Large language models, they seem to do a very decent job of filling in the gaps. Here is one example that I fed to ChatGPT.
So now that we have text extracted from handwritten doctor's reports, custom PDF documents and whatnot, the next step is to extract semantic meaning out of it. I fed this text to Amazon Comprehend Medical and here are the results...
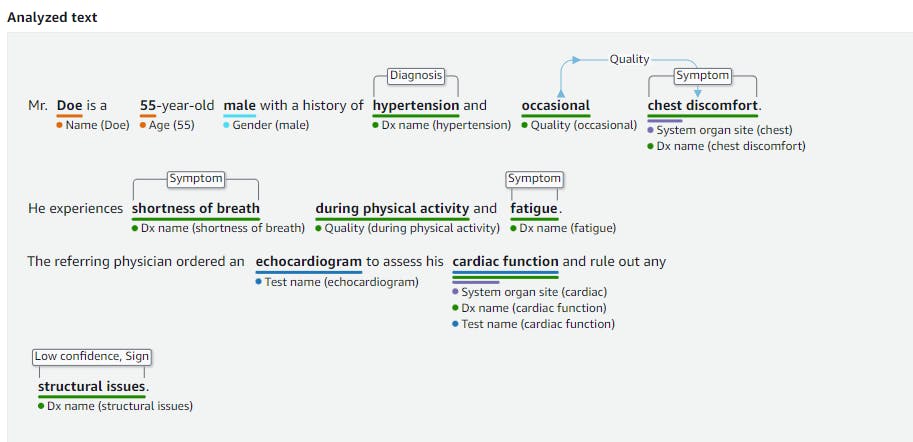
Clinical NLP has extracted entities such as "Diagnosis", "Symptoms", "Age" and "Gender" from free-form text. John Snow Labs claims to be highly accurate for Clinical and BioMedical NLP.
Do you recall Mr. Doe? Our objective was to ensure the Cardiologist received a well-organized and concise summary of all clinically relevant information during Mr. Doe's visit. I think we are almost there.
One option is to present all this information through the Patient Mobile App (See point #1). The other option is to have this information imported into the hospital's Electronic Medical Record.
Healthcare IT unfortunately does not function like FinTech. I can swipe my card issued by Bank X in a Shopping mall, withdraw money from Bank Y ATM, make payments with UPI, and have mortgage deductions from lender Bank Z and all these networks just work! No matter where a transaction originated from it will be reflected accurately in the monthly bank statement.
I briefly spoke about EMR in Part 1. I will explain why consolidating data into an EMR is very important, and the challenges of such a system in the next post.
Disclaimer
This is a personal blog and all the opinions stated in it are my own.
The goal of the current series of blog posts is to talk constructively about how technology can be leveraged to improve lives with a sense of optimism. Demonstrated by examples such as these...
Building a healthcare solution is difficult due to the multifaceted nature of the healthcare domain, stringent regulations, data security concerns, interoperability issues, and the need for clinical validation.
I have intentionally taken a simplified approach to put as many ideas as possible on the table, fostering a vision where healthcare leverages technology to its fullest potential, ultimately benefiting patients in the most innovative ways. Think of it as a Thought Experiment :)
